Case history-8
This is an online e-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
Date of admission:16/11/21
A 39 yr old male came to the opd with the chief complaint of fever and chills since four days ,pain in the abdomen since 4 days , increase frequency of urination since four days .
HISTORY OF PRESENT ILLNESS:
Daily routine :The patient wakes up in the morning at 8am and complete his morning routine and have his breakfast and get ready by 10 am .Then he goes on bike to his working place (cooking master) which is 1km far.He have his lunch at around 1:30-2pm and come home by 3:00-4:00pm and take rest for one hour .have dinner at around 9:30-10 :00pm and goes to sleep by 11:00-12:00am .
The patient was apparently asymptomatic since 3yrs the he went to the hospital with the complaint of increase in frequency of urination and was diagnosed to be type 2 diabetes mellitus and was on regular checkup and since 1month on routine checkup and had uncontrolled sugar >300 and now presented with the compliant of pain in the abdomen at umbilicous and lower abdomen region since 4days not associated with nausea ,vomitings,loose stools .
HISTORY OF PAST ILLNESS:
Complaints of fever ,low grade ,intermittent since 4days .not associated with cough ,cold ,sob ,pedal edema ,palpitation.
TREATMENT HISTORY:
Diabetes-yes (type-2)
No Hypertension,CAD ,asthma ,tuberculosis,antibiotics,hormones ,blood transfusion,surgeries.
PERSONAL HISTORY:
Married
Occupation :cooking master
Decreased appetite,non-vegetarian
Regular bowel movement
Micturation -Burning micturation
No known allergies
Addictions -occasionally
FAMILY HISTORY:
No history of diabetes,hypertension, heart disease, stroke, asthma, tuberculosis,cancers .
General examination:
The patient is conscious, coherent, cooperative.
No Palar
No cyanosis
No lymphadenopathy
No malnutrition
No dehydration
No clubbing
No icterus
No edema
VITALS :
Temp :100 degree F
Pulse rate:86/min
Respiratory rate:26cpm
Bp:150/100mm/hg
Spo2-98%at 8L of o2
Grbs -274mg /dl %
SYSTEMIC EXAMINATION:
CVS :
No thrills
No cardiac murmurs
Cardiac sounds-s1,s2 heard
RESPIRATORY SYSTEM :
No Dysponea
No wheeze
Position of trachea-central
Breath sounds-vesicular
ABDOMEN:
Shape of abdomen-obese
tenderness -at lower abdomen
No palpable mass
Hernial orifices-normal
No free fluid
No bruits
Liver ,spleen-not palpable
Bowel sounds -yes
CNS:
Conscious
Normal speech
No neck stiffness
No kernings signs
Cranial nerves ,motor and sensory system,glasgow scale -normal .
REFLEXES :
Plantars -flexor
CEREBRAL SIGNS:
finger -nose in -coordination -yes
knee -heel in -coordination.-yes
PROVISIONAL DIAGNOSIS:
Acute Pyelonephritis
Acute cystitis
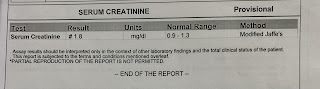
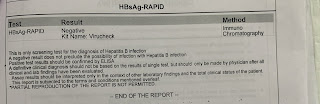
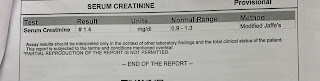
INVESTIGATIONS:
16/11/21:

























Comments
Post a Comment